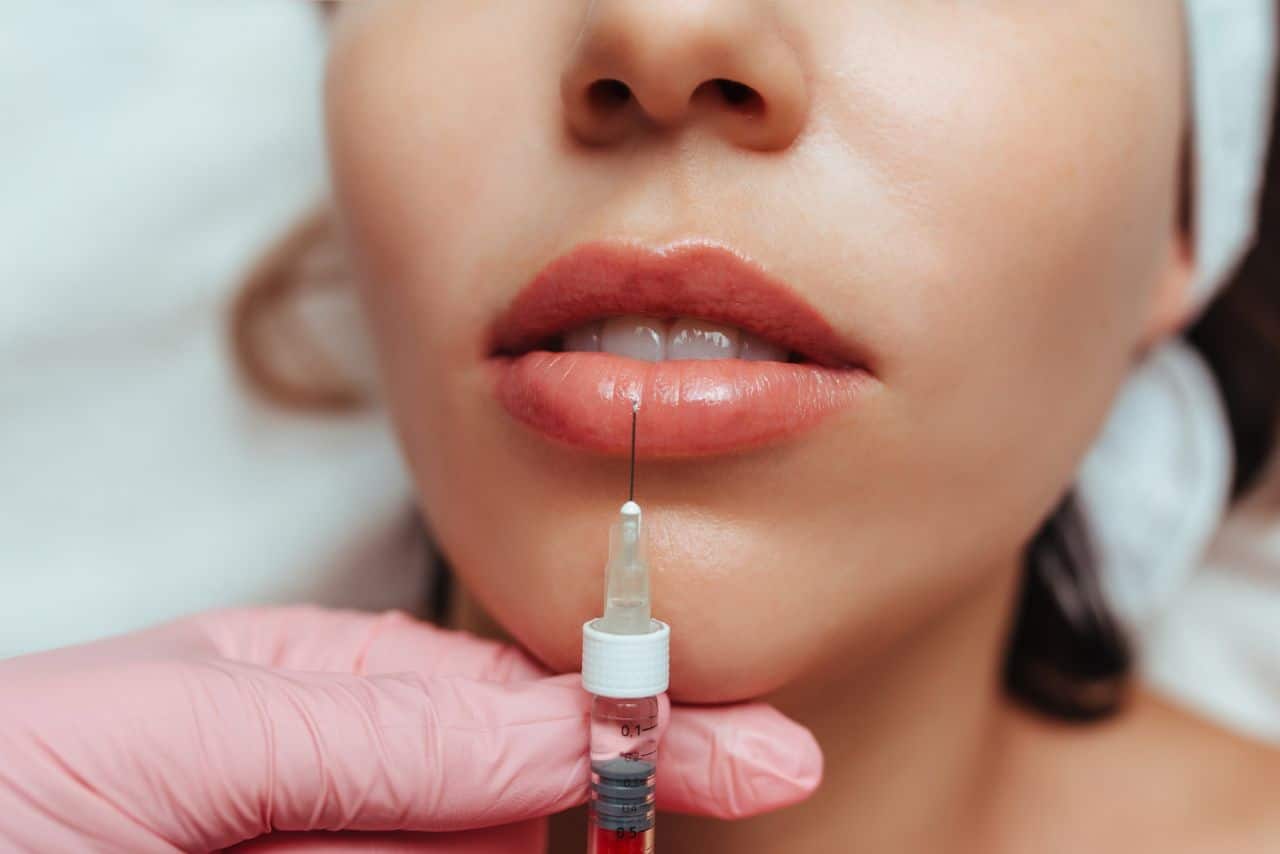
Lip augmentation utilizing dermal fillers, particularly those based on hyaluronic acid (HA), has seen a significant uptick in adoption in aesthetic practice. These procedures’ attractiveness lies in their effective results, relative safety profile, and minimal recovery period. Nonetheless, with their proliferation comes an increase in complications, one of which is lip filler migration. This phenomenon, characterized by the spreading of injected filler material from the initial site of administration to surrounding tissues, presents a considerable challenge in terms of patient satisfaction and aesthetic outcomes.
A thorough understanding of lip filler migration, from its causative factors to its preventive measures and management, is crucial for practitioners to maintain the high standards of care in the evolving landscape of cosmetic dermatology. This article aims to delve into the issue, arming practitioners with the knowledge necessary to minimize risk and effectively handle this complication when it arises.
Understanding Lip Filler Migration
Lip filler migration is a complication that can occur following lip augmentation procedures, predominantly those involving injectable fillers. This phenomenon, while relatively rare when compared to other complications like bruising or swelling, has significant implications on aesthetic outcomes and patient satisfaction.
To mitigate this risk, it is essential for practitioners to have a comprehensive understanding of filler migration and its causes. Lip filler migration occurs when the injected filler substance moves from the original site of placement to surrounding tissues. This migration can lead to visual distortion, yielding lips that appear uneven or asymmetric, and in more extensive cases, alter the overall morphology of the perioral region.
The causes of filler migration are multifaceted and hinges on factors such as the type of filler, injection technique, the anatomic considerations, and individual patient physiology.
Type and Quality of Filler
The rheological properties of the filler – such as its viscosity, elasticity (G’), and cohesivity – significantly influence its likelihood of migration. Fillers with lower viscosity and cohesivity may be more prone to movement within tissue planes. Hyaluronic acid fillers, for instance, can vary in their cross-linking technologies and concentration, altering their physical properties and, in turn, their propensity for migration.
Injection Technique
The expertise and technique of the injector play a pivotal role in filler migration. Injections placed too superficially or with excessive pressure may compromise the structural integrity of tissue planes, promoting filler dispersion. Furthermore, injecting fillers into highly dynamic areas, like the vermilion border, may increase the risk of product displacement due to constant muscular activity.
Anatomic Considerations
The unique anatomy of the perioral region, with its complex interplay of muscles, fat pads, and connective tissue fibers, can influence filler migration. A deep understanding of the anatomical layers, from the dermis to the deeper muscular plane, is necessary to place the filler appropriately and to avoid inadvertent injection into highly mobile or vascular areas.
Patient Physiology
Individual factors such as the patient’s metabolic rate, inherent tissue characteristics, and even certain behaviors or habits (e.g., smoking, high-intensity workout routines, etc.) may influence the longevity and stability of the filler. These factors can also impact the body’s inflammatory response to the filler, possibly accelerating its degradation and leading to early migration or displacement.
Preventing lip filler migration, therefore, requires a precise blend of choosing the right type of filler, employing meticulous injection techniques, understanding the unique anatomy of the lips and surrounding areas, and tailoring the treatment to individual patient characteristics. A comprehensive approach like this ensures that practitioners not only meet the patient’s aesthetic desires but also mitigate the risks associated with the procedure, promoting safer and more satisfying outcomes.
By developing an understanding of lip filler migration, we, as practitioners, can take a proactive approach to anticipate, prevent, and manage this potential complication. In the following sections, we will discuss in greater detail the clinical manifestations of filler migration, strategies to prevent its occurrence, and management plans for cases where migration has occurred.
Awareness and understanding of this complication underline the importance of continuous professional development, training, and up-to-date knowledge in the dynamic field of aesthetic medicine. Even as our tools and techniques evolve, our commitment to patient safety and satisfaction must remain at the core of our practice.

Clinical Manifestations of Filler Migration
Filler migration is a complication that can manifest in various ways, depending on the volume, type of filler used, and the anatomical region where the filler migrates. Importantly, not all instances of migration produce adverse cosmetic outcomes; low-grade, diffuse migration can sometimes contribute to a desirable smoothing effect. However, significant migration can lead to an unnatural appearance, compromised aesthetic results, and patient dissatisfaction.
The lips are a high mobility area, involved in functions like speech, facial expression, and eating. This increased activity may promote the migration of filler materials. In terms of physical appearance, patients with lip filler migration might present with irregularities such as lumps or nodules, asymmetry, or an ‘over-filled’ appearance. This can extend beyond the vermilion border, leading to a ‘duck-like’ lip profile that is commonly associated with overcorrection but can also indicate filler migration.
In more severe cases, the filler may migrate to more distant sites such as the nasolabial folds, marionette lines, or mental crease, leading to an unanticipated volumizing effect in these areas. Beyond the visual manifestations, patients may also report unusual firmness or the sensation of filler material shifting within their lips or surrounding tissues.
Filler migration can also be asymptomatic and detected only on imaging studies such as ultrasound or MRI, performed for other indications. Thus, a high index of suspicion is essential when evaluating a patient who has received lip fillers, especially if they report new or unusual lip or perioral symptoms.
The timing of filler migration can vary widely. In some cases, migration may occur shortly after injection due to the influence of factors such as high injection pressure or injection into highly vascular areas which promote filler dissemination. Alternatively, filler migration might not become apparent until weeks or months post-procedure, especially with repeated treatments, as the cumulative volume of filler can exceed the capacity of the initial treatment area.
When assessing for lip filler migration, it is also important to consider differential diagnoses. The formation of granulomas, foreign body reactions, or localized infections can also cause lip swelling or nodule formation and should be evaluated as potential causes of any presenting symptoms.
The psychological implications of filler migration should not be underestimated. The resulting aesthetic irregularities may cause distress and anxiety for patients, impacting their self-esteem and social interactions. Therefore, a holistic approach to patient care should involve not just addressing the physical manifestations of filler migration, but also providing psychological support and effective communication about the management plan.
Preventing Lip Filler Migration
The prevention of lip filler migration is crucial in ensuring patient satisfaction and minimizing the risk of post-procedure complications. This multifaceted approach involves careful patient selection, refined injection techniques, and the judicious choice of dermal filler.
Patient Selection and Consultation
An effective preventive strategy begins at the consultation stage. Patients should be adequately informed about the potential risks and benefits of the procedure. A detailed medical history, including prior aesthetic procedures, allergies, and underlying health conditions, can reveal contraindications to filler injection or an increased risk of complications such as migration.
Choice of Dermal Filler
Not all dermal fillers are created equal when it comes to the risk of migration. Low-density, non-crosslinked fillers can spread more easily, increasing the likelihood of migration. Therefore, the choice of filler product should be tailored to the individual patient’s lip anatomy, aesthetic goals, and risk profile. Clinicians should consider the rheological properties of fillers, including viscosity, elasticity (G’), and cohesivity, as these can influence the risk of migration.
Hyaluronic acid fillers, given their reversibility and established safety profile, remain a popular choice. Within the class of HA fillers, variations in crosslinking and concentration can influence tissue integration and spread. As a general principle, fillers with higher elasticity and cohesivity may reduce the risk of migration post-injection.
Injection Technique
The skill and technique of the injector are pivotal in preventing filler migration. A deep injection technique, placing the filler directly on the periosteum, can minimize the chance of the filler spreading to surrounding tissues. However, this needs to be balanced against the risk of overcorrection, which can lead to an unnatural appearance.
Understanding the complex anatomy of the perioral region, including the distribution of blood vessels and nerves, is also essential to avoid intravascular injection or nerve injury. Knowledge of the muscular dynamics of the perioral region can guide the strategic placement of filler to resist the pressures of muscular contraction that can lead to product displacement.
Layering techniques, which involve placing a deep bolus followed by superficial threading, may also help to provide a stable scaffold and reduce the chance of filler migration. Practitioners should also consider the total volume of filler used, as higher volumes may increase the likelihood of product displacement.
Post-procedure Guidelines
After the procedure, patients should be instructed to avoid manipulating the treated area for at least 48 hours to prevent the displacement of the filler. Providing patients with clear post-procedure care instructions, including signs of complications such as migration, can enable early detection and intervention.
Continuous Professional Development
To stay abreast of the latest techniques and guidelines in lip augmentation, clinicians should engage in regular professional development and training. Peer-reviewed literature and aesthetic medicine conferences can provide valuable insights into emerging preventive strategies.
By integrating these strategies, clinicians can minimize the risk of lip filler migration, maximizing patient safety, and satisfaction. However, it is crucial to remember that despite all precautions, no procedure is without risk, and a thorough understanding of the management of filler migration is an integral part of aesthetic practice.
Management of Filler Migration
Effective management of lip filler migration requires an astute understanding of the aesthetic goals, initial treatment, and patient’s concerns. Patient reassurance is paramount, emphasizing that treatment options are available and complications are part of the procedural risk.
The first line of management typically involves the use of hyaluronidase products (such as Liporase), an enzyme that metabolizes hyaluronic acid, which constitutes the majority of the dermal fillers used in today’s aesthetic practices. This enzymatic treatment works by breaking down the hyaluronic acid chains in the filler, essentially dissolving it and allowing the body to then naturally eliminate it.
When administering hyaluronidase, caution must be exercised. Overcorrection should be avoided by using small amounts of the enzyme and gradually increasing the dose, always observing the effects before proceeding. Hyaluronidase can diffuse widely, affecting areas beyond the intended site and causing undesired volume loss. Also, since the enzyme works over several hours to days, a waiting period should be observed before re-treatment or re-evaluation.
Moreover, the use of hyaluronidase is not without its potential complications, such as allergic reactions. Although rare, hypersensitivity reactions should be recognized promptly and managed accordingly. An emergency response protocol should always be in place in any aesthetic practice for such scenarios.
In cases where hyaluronidase isn’t applicable or if the filler isn’t based on hyaluronic acid, management becomes more complex. Some fillers are semi-permanent or permanent and don’t respond to enzymatic treatments. For these patients, therapeutic options can include surgical excision, the use of ablative lasers, or even wait-and-see if the body naturally degrades the material over time.
Patient communication is integral throughout the management of filler migration. Patients should be made aware of the possible risks, benefits, and expectations of all corrective measures. They need to understand that the correction process may require several sessions and that the outcome, although likely to be substantial, may not be perfect.
The post-treatment period should be vigilantly monitored, and follow-up appointments scheduled to track the patient’s progress and response to the treatment. It is during these follow-ups that any need for further correction can be assessed and additional treatment planned, if necessary.
On a broader scale, any complication, including filler migration, should be seen as an opportunity for self-auditing. It offers a chance to reflect on one’s own practice and identify potential areas of improvement, whether they lie in the choice of filler, injection technique, patient selection, or aftercare protocols.
Finally, it is essential to report and document all cases of filler migration and their management outcomes. This not only helps in maintaining a high standard of patient care but also contributes to the wider body of research in aesthetic medicine, fostering peer-to-peer learning and ongoing improvements in our field.
Future Directions in Lip Augmentation and Filler Migration
As aesthetic medicine continues to advance, the field of lip augmentation and filler migration also evolves. To provide the highest level of care, physicians need to stay informed about emerging research, innovations, and trends.
Filler Innovations
The development of newer, more advanced fillers is an exciting area of research. Several biotech companies and research institutions are experimenting with different formulations to create products that provide the desired volumizing effect while minimizing the risk of complications such as migration.
One promising avenue is the investigation into the role of filler consistency and cohesivity. These properties impact the filler’s ability to integrate into the tissue and its potential for migration. Research is focused on optimizing these attributes to create fillers that offer superior aesthetic results with fewer complications.
Moreover, advancements in filler ‘reversibility’ represent another promising direction. As of now, hyaluronidase is used to dissolve HA fillers in cases of migration or other complications. However, this is an imperfect solution as it dissolves both migrated and correctly placed filler. The development of fillers that can be selectively ‘turned off’ or removed without affecting the rest of the treatment would mark a significant step forward in the management of filler migration.
Refining Techniques and Approaches
Besides the evolution of filler products, refinement in injection techniques is another area of considerable attention. The concept of a ‘less is more’ approach has gained traction. A move towards more conservative use of fillers, both in terms of volume and frequency, is being advocated. This can potentially reduce the incidence of migration and other complications.
Anatomically tailored treatment plans, which account for variations in individual facial structures and tissue characteristics, may also minimize migration risks. It includes the use of imaging techniques to accurately map the facial anatomy before the injection process. Such a personalized approach ensures the appropriate placement of filler and reduces chances of overcorrection, thereby minimizing the risk of filler migration.
Role of Technology
The role of technology in managing lip augmentation procedures and their potential complications cannot be underestimated. High-definition ultrasound is an emerging tool that has the potential to precisely locate filler placement, identify instances of migration, and help guide the injection of hyaluronidase.
Further, the advancement in AI and machine learning opens up the possibility of predictive analysis. This involves identifying patterns that can predict a higher risk of complications like filler migration, based on a range of variables including patient characteristics, filler type, injection technique, etc. While this is still in its infancy, it holds great potential.
Education and Collaboration
Lastly, the importance of ongoing medical education cannot be overstressed. The exchange of ideas and experiences among clinicians and researchers accelerates the development of best practices. The role of interdisciplinary collaborations and consortiums becomes pivotal in setting standards for lip filler procedures, including techniques to prevent and manage filler migration.
Conclusion
In the evolving world of aesthetic medicine, injectable dermal fillers, particularly hyaluronic acid, have become pivotal in lip augmentation procedures. Their relatively non-invasive nature, coupled with the significant aesthetic outcomes they afford, have contributed to their widespread acceptance. Nevertheless, potential complications like filler migration necessitate a keen understanding and a high level of procedural skill.
Recognizing and navigating the challenges posed by lip filler migration are critical skills in every practitioner’s toolkit, underscoring the importance of ongoing learning and care in clinical practice.

